Introduction to THC
THC is the best-known compound derived from the cannabis plant that makes people feel euphoric, or ‘high’. At the same time, it is also the compound responsible for most of the therapeutic effects attributed to cannabis. THC is shown to decrease nausea and vomiting,
pain, and patient-perceived spasticity (continuous muscle contraction) in
multiple sclerosis (MS), a disease in which the immune system causes degeneration of the neurons.
THC stands for Δ9-tetrahydrocannabinol. The first part is pronounced as delta-nine. The cannabis plant does not directly produce THC. It produces a precursor for THC called THC-acid, or THCA, which does not give you acutely noticeable effects and it does not make you feel high. THCA is converted into THC by a process called decarboxylation (see Figure 1).
1 Typically, this process happens by heating, as explained on our
Decarboxylation Page. This is the reason that before use, cannabis is typically smoked, vaporized, or, when eaten, baked in an oven with cookies or brownies.
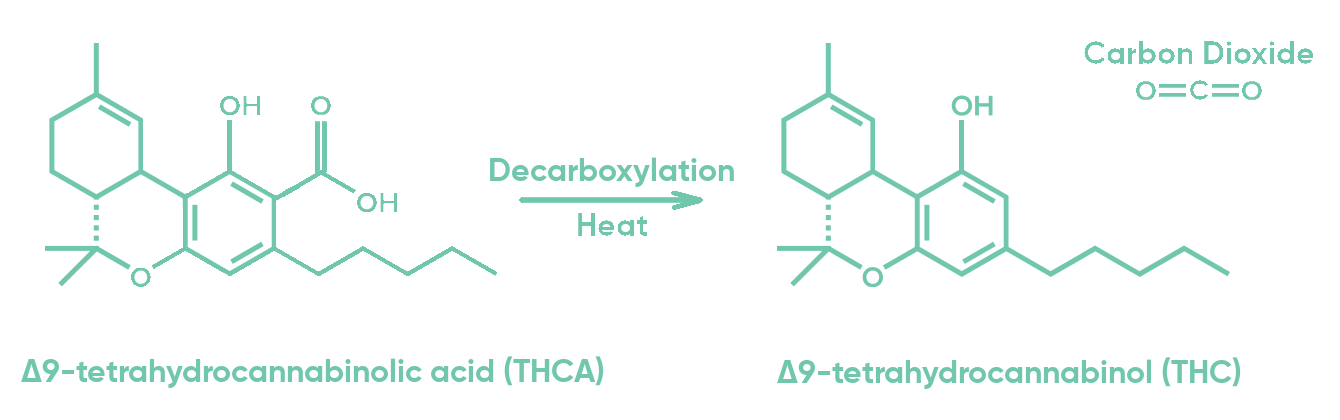 Figure 1: The transformation of THCA molecule into THC + CO2 by heat.
Figure 1: The transformation of THCA molecule into THC + CO2 by heat.
THCA on its own might not have noticeable effects, however, in laboratory studies on the tissue, several potentially therapeutic properties have been identified, including immunity regulation.
2 The therapeutic application in humans of these so-called pre-clinical studies still needs to be investigated.
How does THC work?
THC can enter the body in various ways, and due to its fat-loving nature it will quickly distribute to fatty organs in our body. You can read more about how THC enters and moves around in our body in our
Pharmacokinetics chapter and subchapters.
Receptor binding
THC works on our
endocannabinoid system, which is a physiological system that regulates different processes in our the body. THC induces many of its effects by binding to receptors {call-out, text: Receptors are the structures where molecules can attach to induce their effects.} including
cannabinoid receptors type 1 and 2, or CB1 and CB2. The most well-known effects of THC, such as feeling high, are induced by binding to CB1 (see Figure 2).
3 Although many popular websites describe THC as an agonist on CB1, it is actually a partial agonist, as its binding does not give the full effect (full agonism) that some endocannabinoids can give. For more information about this, including an explanation on what agonism is, click
here.
Upon binding to CB
1, THC modulates the release of molecules that act as messengers between brain cells, called neurotransmitters.
4 The consequences of these actions are the various effects that THC induces.
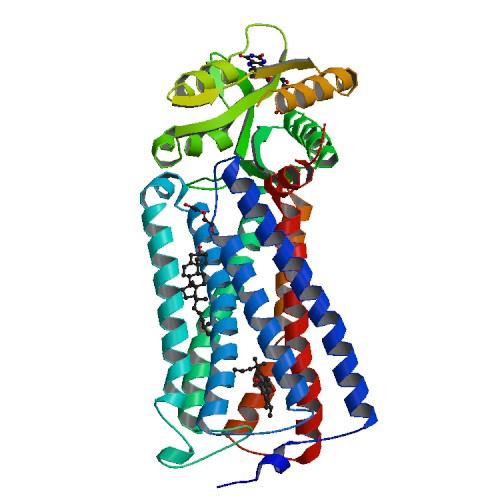 Figure 2: Crystal structure of the human CB1 in complex with agonist AM841 (image taken from IUPHAR/BPS).
11-OH-THC
Figure 2: Crystal structure of the human CB1 in complex with agonist AM841 (image taken from IUPHAR/BPS).
11-OH-THC
Even when pure THC is ingested, THC is not thought to work entirely on its own: in the body, THC is broken down into several compounds called metabolites. One of them, 11-OH-THC (see Figure 3) has been observed to give stronger effects than its parent compound THC.
5 More conversion to 11-OH-THC takes place in the liver after oral THC intake than it does in the lungs after inhalation. Scientists believe that this is why oral THC ingestion gives stronger effects than when the exact same amount of THC is inhaled. For more information about this active metabolite, click
here.
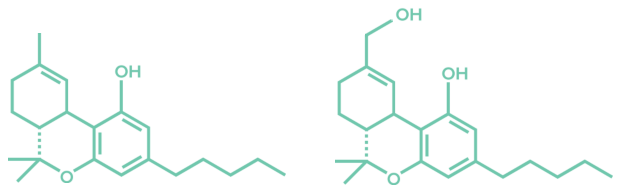 Figure 3: THC and 11-OH-THC molecules.
Figure 3: THC and 11-OH-THC molecules.
Therapeutic effects of THC
On the internet and other media, you can find a lot of information on the therapeutic effects of cannabis or THC in particular, but it is hard to understand which of these sources are reliable. There is a difference between therapeutic claims that have been approved by regulatory agencies for particular drugs, evidence from systematic scientific studies in humans, clues or limited evidence from animal studies or small human studies, and anecdotal stories. Unfortunately, many websites do not explain well where they got their information from. Even medical conditions for cannabis use approved on state levels throughout the US do not explain well why they approve some conditions, but not others. After Cannify’s own review, we saw that some conditions that have scientific evidence for cannabis therapeutic potential are not approved in some states, whereas conditions that have no evidence or sometimes not even a scientific foundation are approved in other studies
6 If you read information online about the therapeutic potential of cannabis, or THC in particular, make sure to understand where the information comes from: look at the exact studies and the proof that one gives.
We’ll try to give you the scientific evidence in a way that is easy to understand. The evidence of therapeutic effects of THC includes the following disorders: chemotherapy-induced nausea and vomiting, anorexia and cachexia {call-out, text: Muscle loss that is associated with an underlying disease such as AIDS or cancer in patients with HIV and AIDS\, chronic and neuropathic pain\, and often in combination with CBD\, MS-related spasticity.}. You can find more information about the studies and outcomes related to these disorders in our chapter
Effects in Health and Disease.
THC has also been shown to decrease intraocular pressure in glaucoma, although the applicability is sometimes debated.
7, 8
THC has been, and currently is, under investigation for many more indications, including treatment of agitation in Alzheimer’s Disease,
9 symptoms in Post Traumatic Stress Disorder (PTSD),
10 and Crohn’s disease.
11
Side effects of THC
Medicinal vs recreational cannabis users
Just as its therapeutic effects, many side effects are to be attributed to THC. Side effects are considered as non-therapeutic effects that are generally unwanted. Patients who seek pain relief to get through their day are unhappy about side-effects such as feeling high. In contrast, recreational users who are not necessarily in search of therapeutic effects to relieve a medical condition, are seeking for these side-effects. This means that there is a difference in the desired goals and sometimes in the perception of what a side-effect means between medicinal and recreational cannabis users.
Acute vs. chronic side effects
Side effects can be divided into acute side effects and chronic side effects. Acute side effects are the side effects that are experienced after a single dose, and typically occur relatively soon after dosing, whereas chronic side effects occur long term after prolonged use.
Acute side effects of THC generally include feeling high or euphoric,
12, 13, 14 drowsiness,
12, 15, 16 dizziness,
15, 16 anxiety,
12, 13, 14, 15, 17 psychotic-like effects,
12, 13, 18 loss of motivation,
13, 18 and an elevated heart rate.
12, 14, 16, 19 18, 20 All side-effects are dose-dependent, which means that a higher dose gives a stronger effect. High doses are also associated with fainting.
Chronic side effects associated with THC can include: depression,
12, 13, 15, 21, 22 psychosis,
12, 13, 18 and cannabis use disorder, or CUD, which is a cannabis dependency.
7, 23, 24 Another side effect that occurs in some individuals is Cannabis Hyperemesis Syndrome, or CHS, during which the patient gets nausea and vomiting after the use of cannabis products.
25, 26 The only way to stop these symptoms is to stop using cannabis products. Chronic side-effects are generally associated with the age at the onset of use: the younger the patient is at first cannabis use, the more likely they are to develop or trigger chronic side effects such as depression or psychosis.

If you want to learn more about cannabis and safety, click
here.
Besides THC, CBD is the second major cannabinoid. You can read more about it on the
Introduction to CBD page.
- Veress, T.; Szanto, J. I.; Leisztner, L. (1990). Determination of cannabinoid acids by high-performance liquid chromatography of their neutral derivatives formed by thermal decarboxylation: I. Study of the decarboxylation process in open reactors. Journal of Chromatography A, 520(Supplement C), 339--347.
- Verhoeckx, Kitty C. M.; Korthout, Henrie A. A. J.; van Meeteren-Kreikamp, A. P.; Ehlert, Karl A.; Wang, Mei; van der Greef, Jan; Rodenburg, Richard J. T.; Witkamp, Renger F. (2006). Unheated Cannabis sativa extracts and its major compound THC-acid have potential immuno-modulating properties not mediated by CB1 and CB2 receptor coupled pathways. International immunopharmacology, 6(4), 656--665.
- Klumpers, Linda E.; Fridberg, Marianne; de Kam, Marieke L.; Little, Paul B.; Jensen, Niels Ole; Kleinloog, Hendrik D.; Elling, Christian E.; van Gerven, Joop M. A. (2013). Peripheral selectivity of the novel cannabinoid receptor antagonist TM38837 in healthy subjects. British Journal of Clinical Pharmacology, 76(6), 846--857.
- Colizzi, Marco; McGuire, Philip; Pertwee, Roger G.; Bhattacharyya, Sagnik (2016). Effect of cannabis on glutamate signalling in the brain: A systematic review of human and animal evidence. Neuroscience & Biobehavioral Reviews, 64, 359-381.
- Lemberger, Louis; Crabtree, Ross E.; Rowe, Howard M. (1972). 11-Hydroxy-delta9-tetrahydrocannabinol:-Pharmacology, Disposition, and Metabolism of a Major Metabolite of Marihuana in Man. Science, 177, 11--13.
- Klumpers, Linda; Boncales, Danica (2020). Conditions per State.
- National Academies of Sciences, Engineering, and Medicine (2017). The Health Effects of Cannabis and Cannabinoids. Nap 24625 (440). National Academies Press.
- Hergenrather, Jeffrey (2019). Cannabis as a treatment for glaucoma.
- Rosenberg, Paul; Forester, Brent P. (2016). Trial of Dronabinol Adjunctive Treatment of Agitation in Alzheimer's Disease (AD) (THC-AD) (THC-AD). https://clinicaltrials.gov/ct2/show/NCT02792257.
- Shalev, Arieh Y. (2009). Add on Study on Δ9-THC Treatment for Posttraumatic Stress Disorders (PTSD) (THC_PTSD). https://clinicaltrials.gov/ct2/show/NCT00965809.
- Meir Medical Center (2013). Combined THC and CBD Drops for Treatment of Crohn's Disease. https://clinicaltrials.gov/ct2/show/NCT01826188.
- Karila, Laurent; Roux, Perrine; Rolland, Benjamin; Benyamina, Amine; Reynaud, Michel; Aubin, Henri-Jean; Lancon, Christophe (2014). Acute and long-term effects of cannabis use: a review. Current pharmaceutical design, 20(25), 4112--4118.
- Johns, A. (2001). Psychiatric effects of cannabis. The British journal of psychiatry : the journal of mental science, 178, 116--122.
- Hall, Wayne; Solowij, Nadia (1998). Adverse effects of cannabis. The Lancet, 352(9140), 1611--1616.
- Green, Bob; Kavanagh, David; Young, Ross (2003). Being stoned: a review of self-reported cannabis effects. Drug and alcohol review, 22(4), 453--460.
- Borgelt, Laura M.; Franson, Kari L.; Nussbaum, Abraham M.; Wang, George S. (2013). The pharmacologic and clinical effects of medical cannabis. Pharmacotherapy, 33(2), 195--209.
- Hall, Wayne (2009). The adverse health effects of cannabis use: What are they, and what are their implications for policy?. International Journal of Drug Policy, 20(6), 458--466.
- Hollister, Leo E. (1986). Health aspects of cannabis. Pharmacological reviews, 38(1), 1--20.
- Jones, Reese T. (2002). Cardiovascular system effects of marijuana. Journal of clinical pharmacology, 42(S1), 58S--63S.
- Beaconsfield, Peter; Ginsburg, Jean; Rainsbury, Rebecca (1972). Marihuana Smoking. New England Journal of Medicine, 287(5), 209--212.
- Lynskey, Michael T.; Glowinski, Anne L.; Todorov, Alexandre A.; Bucholz, Kathleen K.; Madden, Pamela A. F.; Nelson, Elliot C.; Statham, Dixie J.; Martin, Nicholas G.; Heath, Andrew C. (2004). Major Depressive Disorder, Suicidal Ideation, and Suicide Attempt inTwins Discordant for Cannabis Dependence and Early-Onset Cannabis Use. Archives of General Psychiatry, 61(10), 1026.
- Bahorik, Amber L.; Leibowitz, Amy; Sterling, Stacy A.; Travis, Adam; Weisner, Constance; Satre, Derek D. (2017). Patterns of marijuana use among psychiatry patients with depression and its impact on recovery. Journal of Affective Disorders, 213, 168--171.
- Cougle, Jesse R.; Hakes, Jahn K.; Macatee, Richard J.; Zvolensky, Michael J.; Chavarria, Jesus (2016). Probability and correlates of dependence among regular users of alcohol, nicotine, cannabis, and cocaine: concurrent and prospective analyses of the National Epidemiologic Survey on Alcohol and Related Conditions. The Journal of clinical psychiatry, 77(4), e444--50.
- Chen, Chuan-Yu; O'Brien, Megan S.; Anthony, James C. (2005). Who becomes cannabis dependent soon after onset of use? Epidemiological evidence from the United States: 2000–2001. Drug and Alcohol Dependence, 79(1), 11--22.
- Allen, J. H.; de Moore, G. M.; Heddle, R.; Twartz, J. C. (2004). Cannabinoid hyperemesis: cyclical hyperemesis in association with chronic cannabis abuse. Gut, 53(11), 1566--1570.
- Sontineni, Siva P.; Chaudhary, Sanjay; Sontineni, Vijaya; Lanspa, Stephen J. (2009). Cannabinoid hyperemesis syndrome: clinical diagnosis of an underrecognised manifestation of chronic cannabis abuse. World journal of gastroenterology, 15(10), 1264--6.
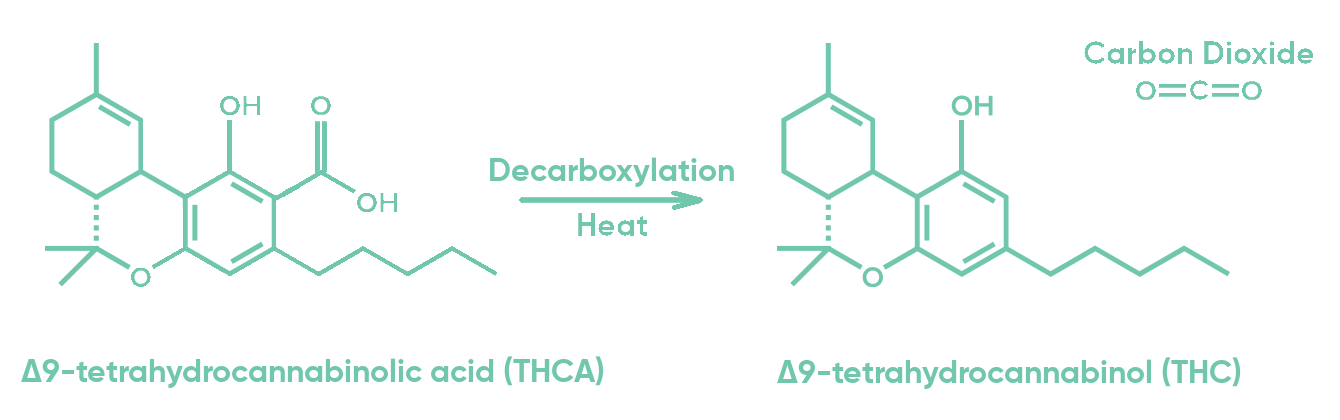 Figure 1: The transformation of THCA molecule into THC + CO2 by heat.
THCA on its own might not have noticeable effects, however, in laboratory studies on the tissue, several potentially therapeutic properties have been identified, including immunity regulation.2 The therapeutic application in humans of these so-called pre-clinical studies still needs to be investigated.
Figure 1: The transformation of THCA molecule into THC + CO2 by heat.
THCA on its own might not have noticeable effects, however, in laboratory studies on the tissue, several potentially therapeutic properties have been identified, including immunity regulation.2 The therapeutic application in humans of these so-called pre-clinical studies still needs to be investigated.
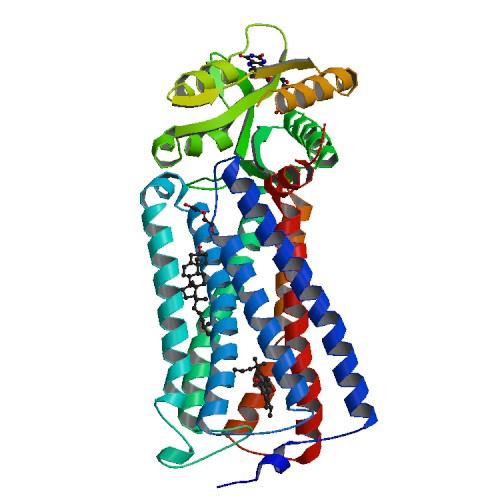 Figure 2: Crystal structure of the human CB1 in complex with agonist AM841 (image taken from IUPHAR/BPS).
11-OH-THC
Even when pure THC is ingested, THC is not thought to work entirely on its own: in the body, THC is broken down into several compounds called metabolites. One of them, 11-OH-THC (see Figure 3) has been observed to give stronger effects than its parent compound THC.5 More conversion to 11-OH-THC takes place in the liver after oral THC intake than it does in the lungs after inhalation. Scientists believe that this is why oral THC ingestion gives stronger effects than when the exact same amount of THC is inhaled. For more information about this active metabolite, click here.
Figure 2: Crystal structure of the human CB1 in complex with agonist AM841 (image taken from IUPHAR/BPS).
11-OH-THC
Even when pure THC is ingested, THC is not thought to work entirely on its own: in the body, THC is broken down into several compounds called metabolites. One of them, 11-OH-THC (see Figure 3) has been observed to give stronger effects than its parent compound THC.5 More conversion to 11-OH-THC takes place in the liver after oral THC intake than it does in the lungs after inhalation. Scientists believe that this is why oral THC ingestion gives stronger effects than when the exact same amount of THC is inhaled. For more information about this active metabolite, click here.
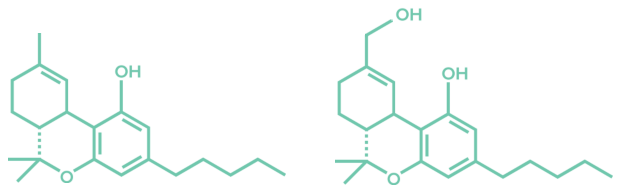 Figure 3: THC and 11-OH-THC molecules.
Figure 3: THC and 11-OH-THC molecules.
 If you want to learn more about cannabis and safety, click here.
Besides THC, CBD is the second major cannabinoid. You can read more about it on the Introduction to CBD page.References:
If you want to learn more about cannabis and safety, click here.
Besides THC, CBD is the second major cannabinoid. You can read more about it on the Introduction to CBD page.References:_logo.svg)